Straumann Pro Arch Rehabilitation of the Edentulous Maxilla
submitted by:
Richard Kinsel DDS
Bryan Pope DMD MSD
Daniele Capoferri
Share This


A forty-six year old female presented to our clinic with advanced caries of her maxillary teeth. All of the teeth were considered non restorable and terminal. She had a combination of metal ceramic crowns and a flexible removable partial denture that replaced her missing teeth. Masticatory function and appearance were adversely affected (Fig. 1 & Fig. 2). The patient was healthy and a nonsmoker with no medical contraindications to implant treatment. Her treatment goal was a cost effective and long-term, predictable implant-supported fixed solution that could replace her debilitated dentition.
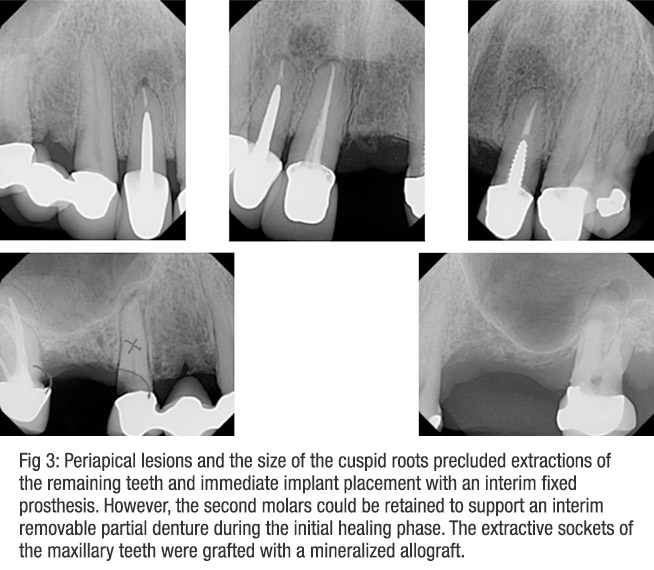
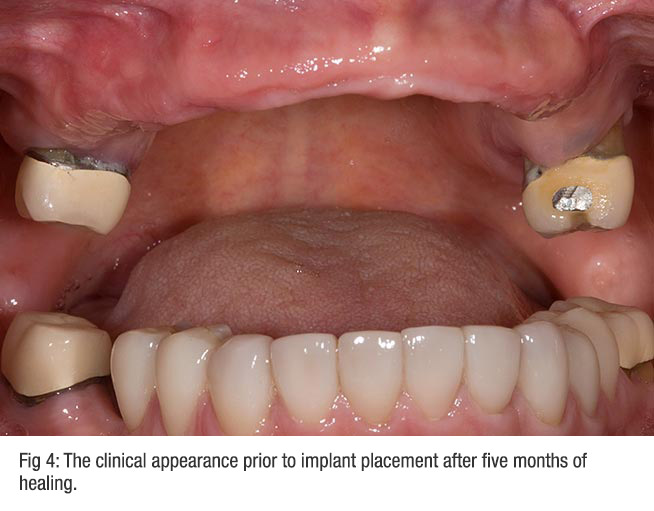
Periapical lesions and large root diameters at prospective implant sites precluded the extraction, immediate implant placement, and restoration of the maxillary arch (Fig 3). However, the carious second molars could serve as support for an interim removable partial denture. These teeth would be removed following delivery of the definitive implant-supported prosthesis. The remaining maxillary teeth (with the exception of the second molars) were extracted and the future implant sites grafted with a mineralized allograft (Fig 4).
After five months, a radiographic guide was fabricated by duplicating the interim partial denture in clear acrylic resin with a facial flange added for stability. A dual scan was completed of the maxillary arch and radiographic guide. The DICOM images were imported into an implant planning software and reviewed by the treatment team.
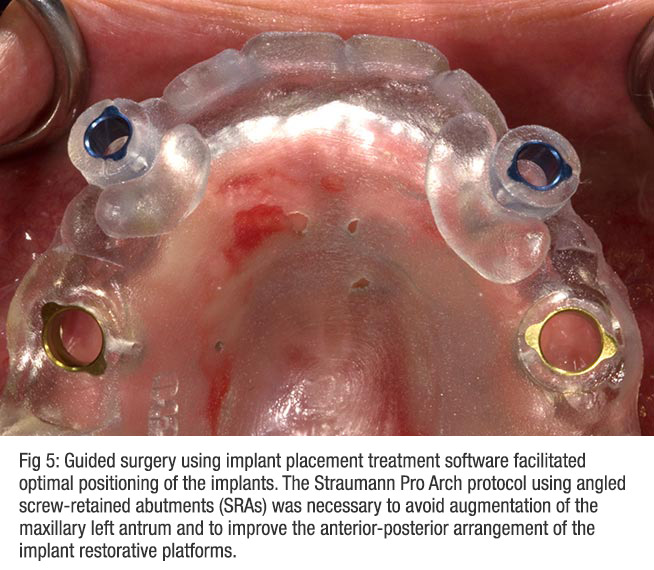
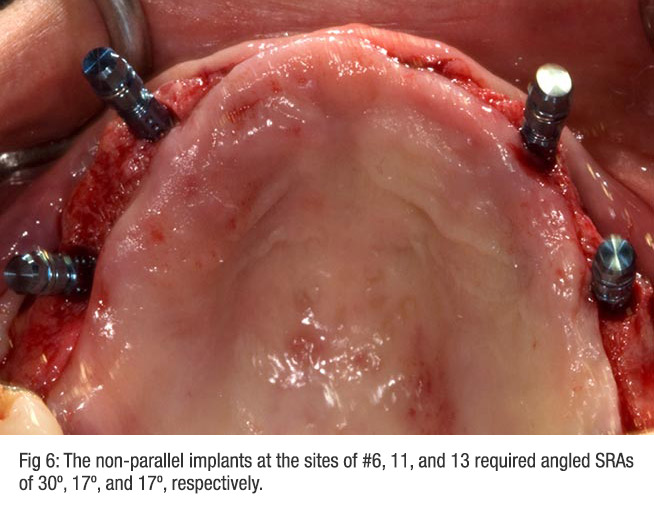
The angulation of the upper left second premolar implant was distalized to avoid the left antrum while maximizing the anterior-posterior dimension of the final prosthesis. This angulation combined with a significant osseous undercut in the premaxilla required restorative angle correction of 3 out of the 4 implants. Straumann® Screw-Retained abutments (SRAs) were chosen to parallel the maxillary left premolar (17º) and cuspid (17º and 30º) implants. A surgical guide was fabricated from the treatment planning software to facilitate optimal implant positioning (Fig 5).
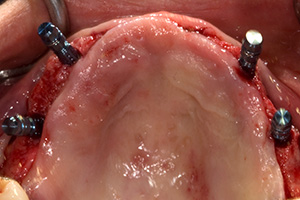
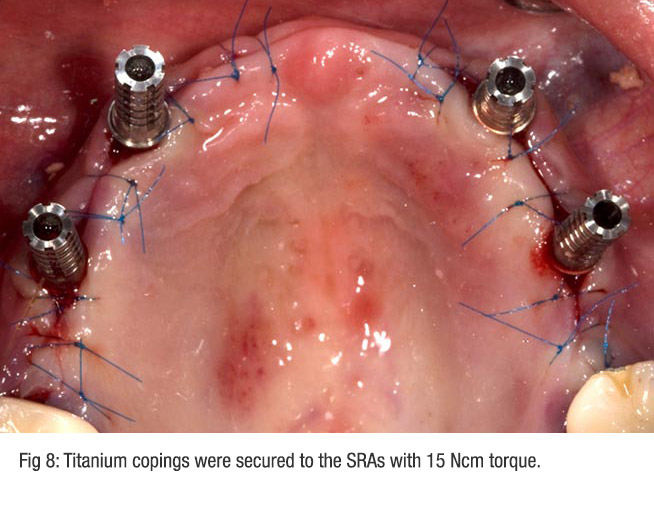
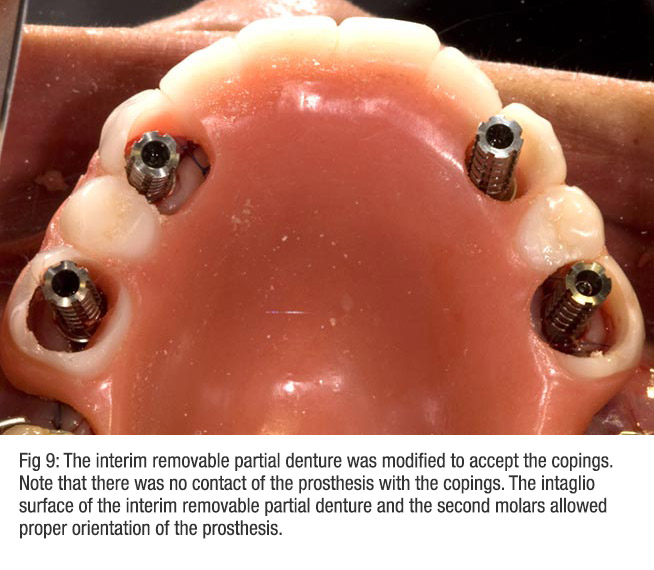
The implant team was present at the implant/restorative appointment. Straumann® Bone Level RC implants (10mm) were placed at the second premolar sites and NC implants (12mm) at the cuspid sites (Fig 6). All implants were Roxolid™ with favorable initial stability confirmed by the surgeon. The straight and angled SRAs that had been chosen from the implant treatment planning software were inserted and the wound approximated and sutured (Fig 7). Titanium copings were placed on the SRAs (Fig 8). The interim partial denture was modified to accept the cylinders (Fig 9).
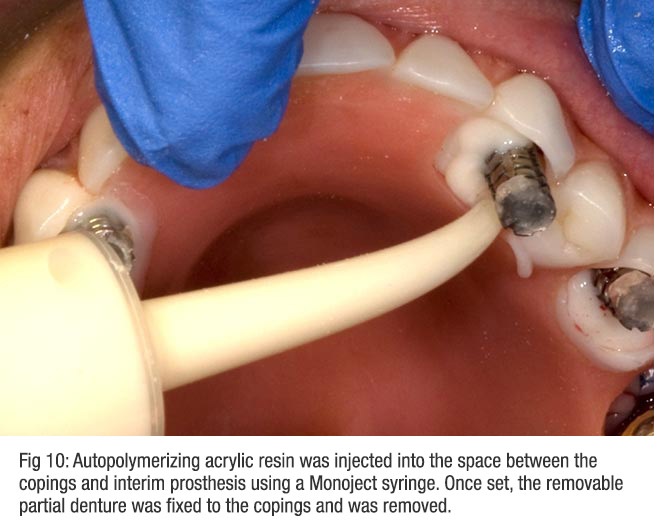
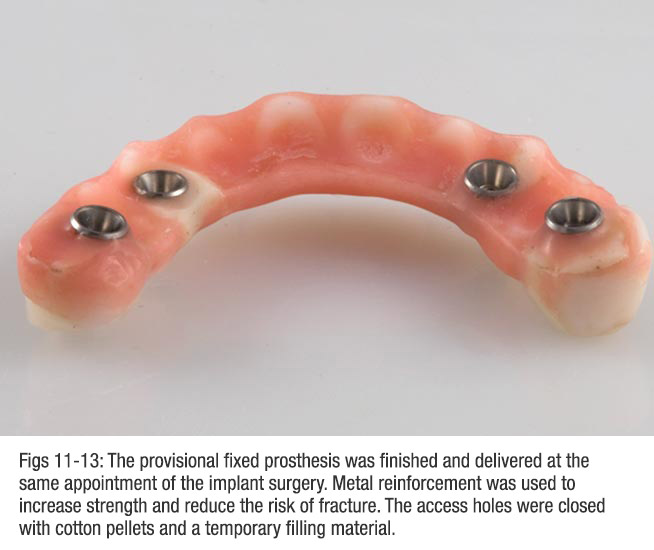
The sutures were lubricated with Vaseline® and autopolymerizing acrylic resin was injected with a Monoject irrigation syringe to connect the cylinders to the interim prosthesis (Fig 10). The intaglio surface and the clasps that engaged the second molars ensured proper orientation of the prosthesis. The facial and palatal acrylic was removed. The intaglio surface was corrected and the prosthesis finished (Fig 11).
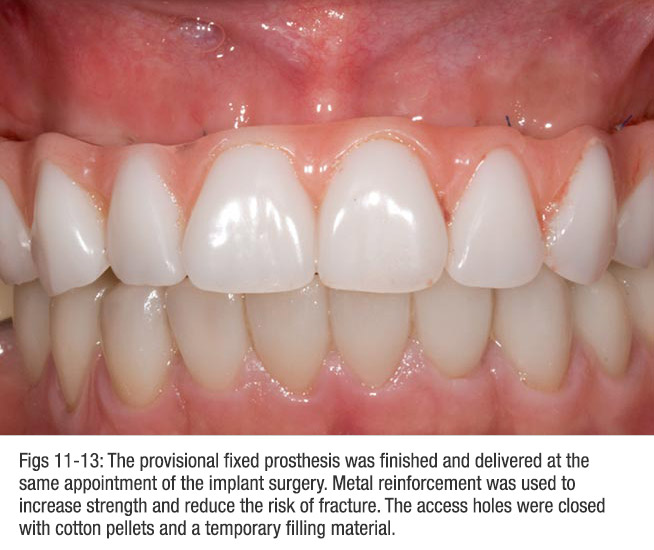
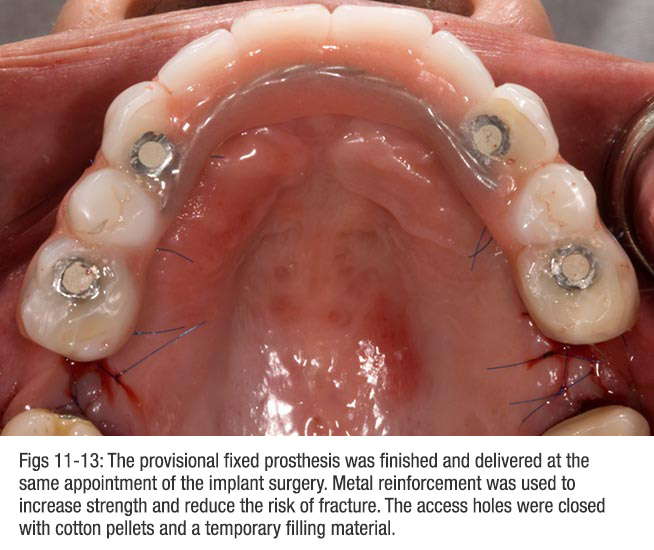
The implant-supported provisional prosthesis was affixed to the SRAs. The intaglio surface was relieved to prevent impingement on the soft tissue from the anticipated postsurgical swelling (Fig 12). The provisional prosthesis was reinforced with metal to reduce the risk of fracture and the occlusal access holes were closed with cotton pellets and a temporary filling material (Fig 13).
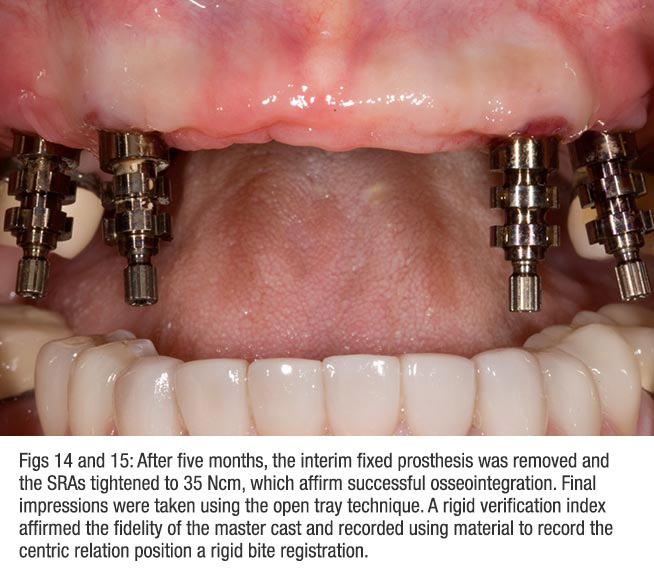
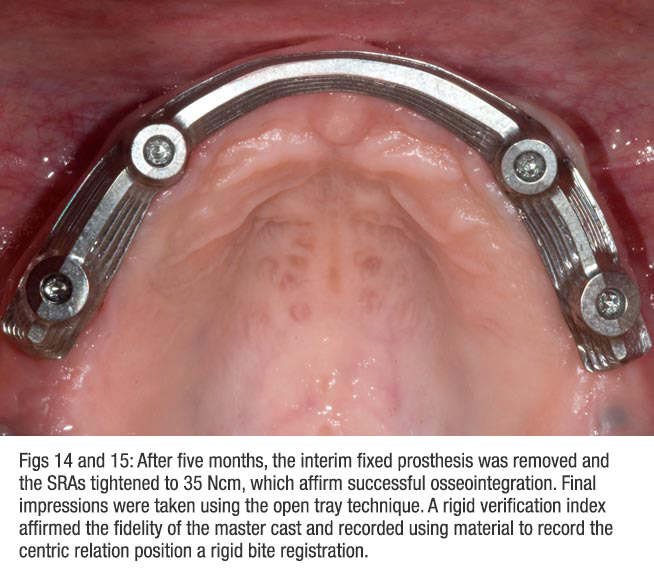
After two months, the prosthesis was removed and the SRAs were torqued to 35 Ncm, generally considered consistent with successful implant osseointegration. The final impression was taken using a polyvinylsiloxane material and the open tray technique (Fig 14). The fidelity of the master cast to the in situ implant positions was confirmed with an index that connected the titanium temporary abutments with laboratory burs and dimensionally stable autopolymerizing acrylic resin. This same index also served to record the centric relation position using a rigid bite registration material.
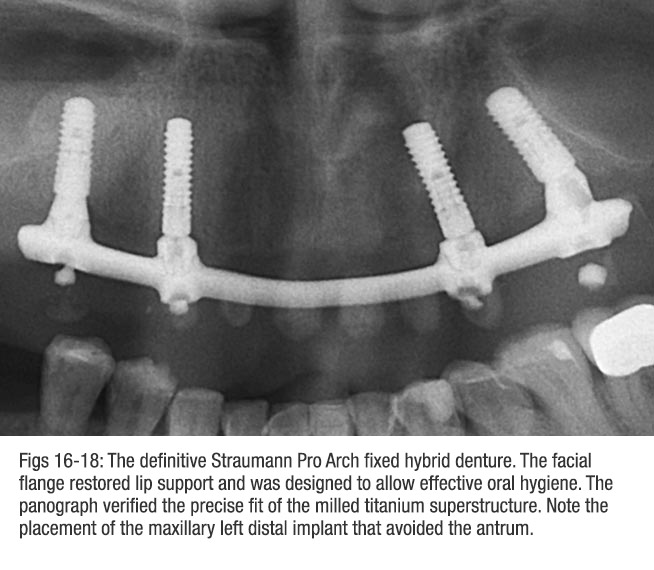
The master cast with denture teeth setup was sent to Straumann's CARES® Scan & Shape Service to be scanned. It is important to have pristine laboratory abutments in the master case. The restorative dentist and laboratory technician approved the prospective design for the titanium substructure. The milled Advanced Fixed Bar bar was inserted (Fig 15) and the fit on the implants was confirmed by radiographs (Fig 16).
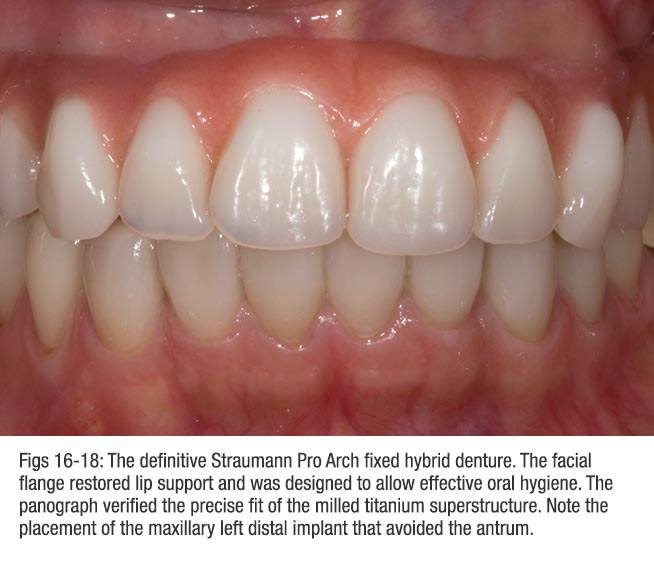
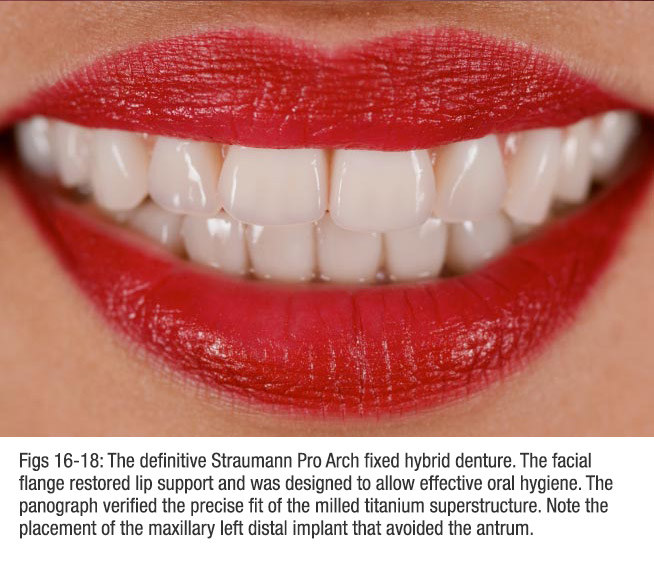
The definitive Straumann Pro Arch fixed hybrid denture required a facial flange (façade) to mask the transition from the denture acrylic and gingival mucosa (Fig 17). The prosthesis was designed to facilitate oral hygiene, especially the use of spongy-type floss for the intaglio surface (Oral-B Super Floss®, P&G Co, Cincinnati, OH). The final result restored optimal esthetics and function (Fig 18).
The surgeon's placement of the SRAs was facilitated by direct observation provided by the reflected tissue. The modification of the interim removable prosthesis to accept the temporary cylinders was straightforward. Connection of the cylinders to the prosthesis with autopolymerizing acrylic resin ensured passivity.
Importantly, the CARES® milled titanium bar consistently fits the master cast. Therefore, the restorative team must verify the cast with the in situ implant positions prior to forwarding to the CARES®® dental laboratory. If this is not done and the master cast is not accurate, a new impression and confirmation index would be needed. This would result in increase treatment time with patient and dentist frustration.
The Straumann Pro Arch protocol using screw-retained abutments was particularly well suited for this patient’s challenges—premaxilla facial inclination, avoiding left antrum bone grafting, and establishing a favorable anterior-posterior arrangement of the implant restorative platforms. The benefits include improved masticatory function and appearance immediately following surgery, no sinus bone augmentation, reduced treatment time, and reduced cost.
Generally, we can complete the implant surgery and provisional fixed restoration in less than four hours. Patients remark that there is little to no post-surgical discomfort. They are pleased with a collaborative approach and more comfortable with a known treatment team in a private practice setting.



Richard P. Kinsel, DDS
Fellow, Academy of Osseointegration
Fellow, International Team for Implantology
Private Practice Foster City, CA

Bryan I Pope, DMD, MSD
Private Practice San Mateo, CA

Daniele Capoferri
Oral Design® Member