Double Jaw Immediate Load Hybrids: Case Abstract
submitted by:
Scott E. Keith, DDS, MS
John J. Petrini, DDS, MS
Share This


A 56 year-old male patient was referred to our specialty private practice in August of 2014 for an evaluation and consultation to determine if he would be a candidate for treatment with Dental Implants. The patient's main concerns included multiple missing teeth, dissatisfaction with his smile and gradually increasing difficulty eating certain foods. He did also report that he had recently noticed his teeth becoming looser and an inability to wear a maxillary removable partial denture due to an extreme gag reflex. He was able to wear a mandibular removable partial denture but found it uncomfortable and only used it when out in public, at work and in social situations. He was told by his General Dentist of more than 20 years that he was not a candidate for dental implants due to his smoking habit of about 1 pack per day for more than 25 years. He was in fairly good overall health and managed his borderline hypertension with diet and mild exercise. In fact, he had managed to quit smoking in the prior year and was very motivated to seek dental treatment to replace his failing teeth and removable partial dentures with fixed, implant supported hybrid restorations.
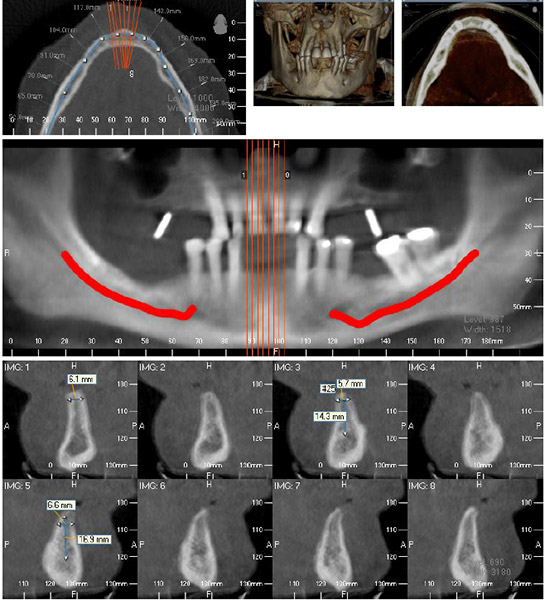
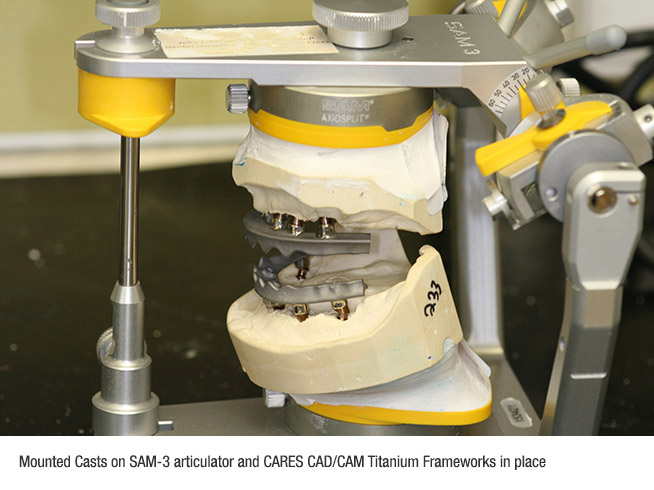
After a complete history and clinical examination were completed, diagnostic alginate impressions and photographs were obtained (Fig. 1 & Fig. 2). The patient made clear during his initial visit and throughout the treatment planning process that he would not be able to tolerate conventional complete removable dentures at any stage of treatment. He had thoroughly researched some potential treatment options online, and specifically sought out our office with the desire to receive immediate load provisional hybrids the same day his teeth were removed. His diagnostic study casts were mounted on a SAM-3 articulator with a facebow transfer and evaluated for skeletal relationship, basal alveolar bone, and potential ideal tooth position. A cone beam CT Scan was obtained to evaluate bone quantity and quality in both arches (Fig. 3.a & Fig. 3.b). A three -dimensional reformat of the patient's maxillary and mandibular anatomy allowed for identification of available bone volume for implant placement in both jaws to maximize implant distribution and support and avoid vital structures including the inferior alveolar nerves and maxillary sinuses and nasal floor. Informed consent was obtained for removal of all remaining teeth under local anesthetic with conscious sedation and placement of 5 to 6 implants in each arch. In addition, the goal of treatment that day included fabrication of immediate load fixed provisional hybrids to provide the patient with a complete dentition.
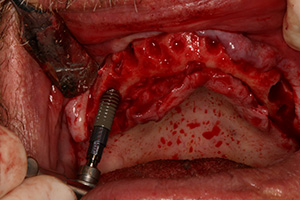
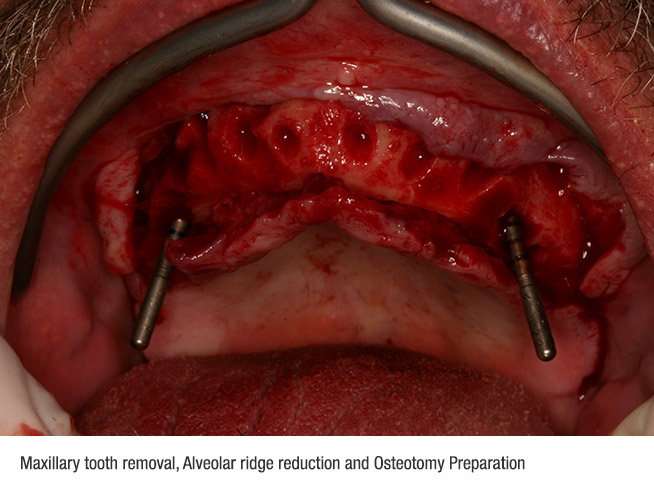
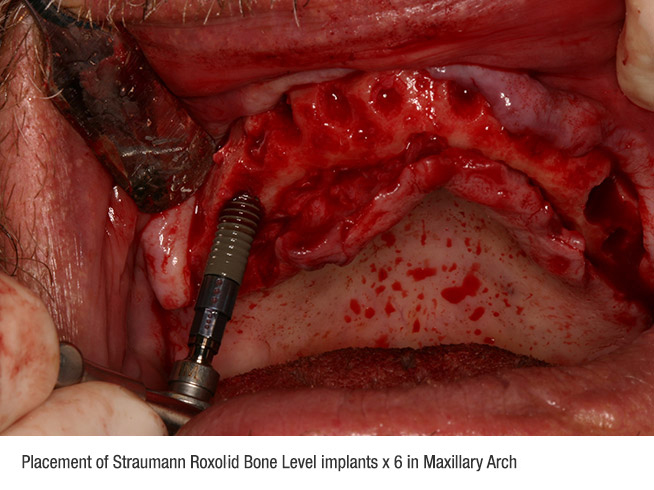
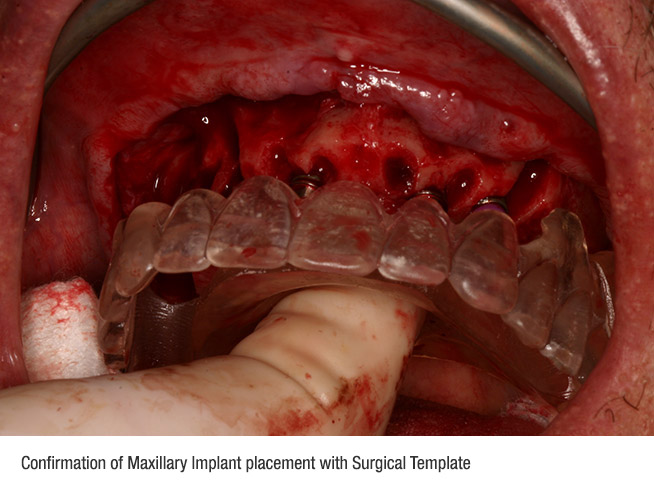
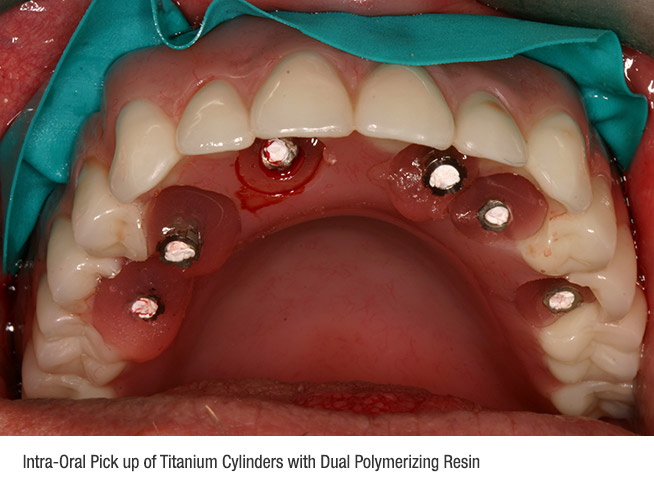
His wife escorted the patient to our office on the day of surgery. The patient's vital signs were monitored throughout the procedure and treatment was initiated in the maxillary arch. After reflection of a muco-periosteal flap, the six remaining upper teeth were removed. The crestal alveolar bone was removed with a straight surgical handpiece under copious sterile saline irrigation. Upon completion of the maxillary ostectomy, preparation of the distal implant osteotomy sites was initiated (Fig. 4). These distal implant sites were tilted to avoid the anterior wall of the maxillary sinuses yet maximize the amount anterior-posterior implant distribution (Fig. 5). Implant site preparation and final placement was confirmed with the assistance of a clear surgical template (Fig. 6). A total of six Straumann Bone Level RC Roxoloid implants were placed in the maxilla with insertion torque between 35-55 Ncm. In order to achieve placement of screw access hole location in ideal prosthetic positions for the prosthesis, three 17° angled and three straight SRA (screw-retained abutments) were placed using 35 Ncm of torque on the abutment screws (Fig. 7). Any residual extraction socket defects were grafted with Straumann Allograft large particle cortico-cancellous mix and the gingival flaps were closed with 4.0 Chromic Gut interrupted sutures. A maxillary complete denture was then inserted over the abutments and protective caps to transfer position of screw access hole locations to the prosthesis (Fig. 8). Titanium copings for the SRA abutments were attached at 15 Ncm to confirm proper modification of the denture. Teflon tape was placed into the titanium copings and a non-latex dental dam was cut to size and placed over the copings in preparation for an intra-oral pick up of the cylinders (Fig. 9). A dual polymerizing resin (Triad DuaLine) was placed in the denture and injected around the copings to firmly index and attach the titanium copings within the denture. The maxillary prosthesis was disinfected and taken into the in-house laboratory for conversion into a fixed provisional Hybrid.
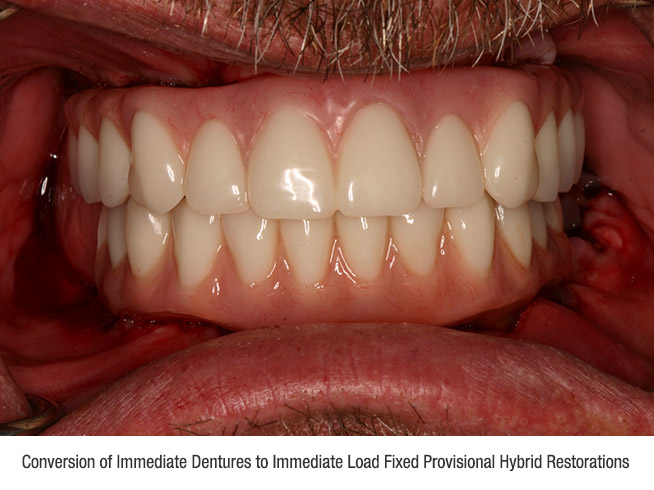
The patient was then given some time to use the restroom and consume a small protein shake. After this brief stretch break, the patient was again prepared under sterile surgical drapes for treatment of the mandibular arch. After delivery of local anesthetic, the lower teeth were removed, the alveolar shelf was prepared and five implants were placed according to the same protocol described above. Three straight and two angled (one 17degree and one 30 degree) SRA abutments were placed at 35 Ncm. The converted maxillary hybrid was delivered on the abutments with prosthetic screws at 15 Ncm to allow a reference for orientation of the lower denture. A mandibular complete denture was then indexed and copings were picked up in the same manner as the maxillary arch. The mandibular prosthesis conversion was completed in the same approach to create a highly polished tissue surface with cleansable contours and minimal cantilever length to minimize fracture potential in the healing phase. The screw-access holes were closed with Teflon tape and Telio soft setting composite resin. The occlusion was evaluated with a T-Scan digital occlusal analyzer and adjusted to achieve evenly distributed occlusal contacts, accurately eliminate interferences, and confirm proper bite force around the arches. Post-operative written instructions were reviewed with the patient and his wife. They were reminded for the patient to adhere to an extremely soft diet the first 6 weeks. The patient was thrilled to leave the office that day with a complete dentition (Fig. 10).
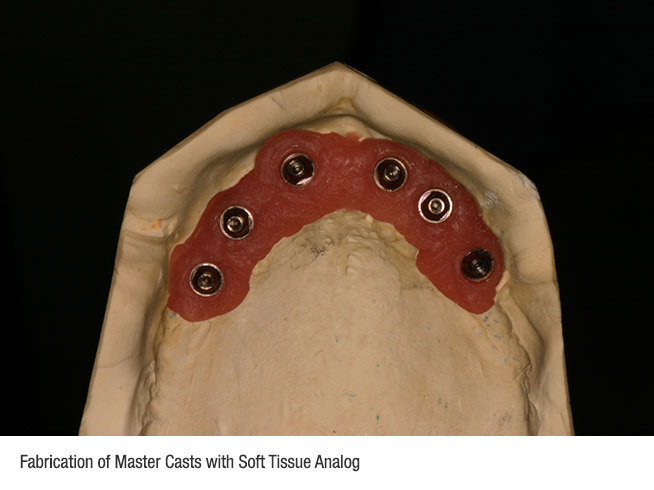
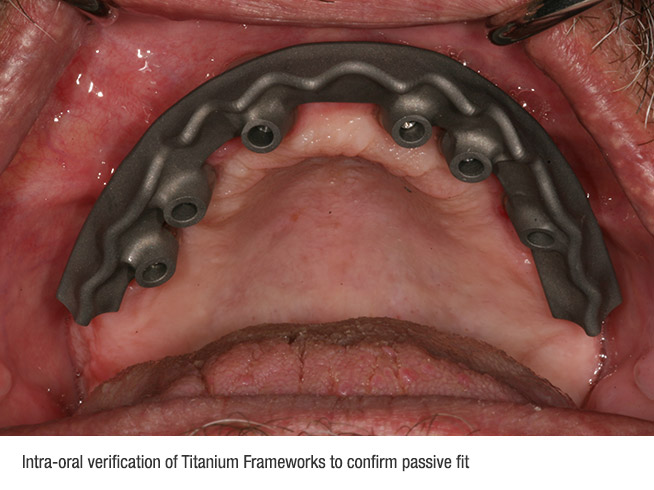
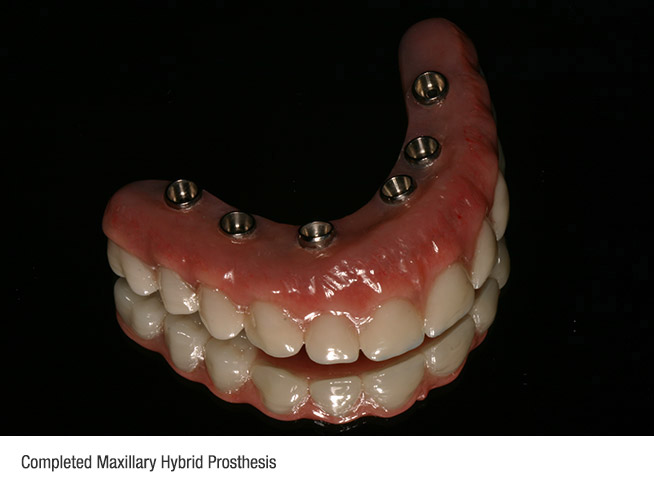
The patient was seen for a series of follow up appointments to evaluate healing over the first 2 months. Peri-apical radiographs were made at 8 weeks post-op at which time the patient was instructed to begin using an oral irrigator on a low setting to better clean the tissue surface of the hybrids. After 5 months of uneventful healing, the patient was brought back to begin fabrication of the final prostheses. The fabrication of the final hybrid restorations usually requires a series of 5 one-hour appointments, which usually do not require the administration of local anesthetic. The screw-access hole fillings were removed and both provisional hybrids were removed. All abutment screws were checked to confirm and tighten at 35 Ncm. Open tray SRA impression copings were placed over the abutments and final full arch impressions were made with a Polyvinylsiloxane material (Fig. 11). Master casts were poured using SRA analogs and a soft tissue moulage material (Fig. 12). The casts were then mounted using the patient's provisional hybrids during the second clinical appointment. A tooth set up on wax rims was tried in to verify esthetics and phonetics at the third clinical appointment to confirm tooth position. The dental laboratory then digitized the verified tooth and implant positions in the Straumann CS2 scanner. Using the CARES software, the technician designed the CAD/CAM titanium bar to precisely fit the implant abutments and support the final denture teeth in the permanent prostheses (Fig. 13). The CARES titanium bars were tried in to verify passive fit on the implant abutments prior to final processing (Fig. 14). The teeth were then transferred to the bars in the laboratory using a putty matrix of the confirmed tooth position for one final try in. The hybrids were then returned to the lab for opaquing of the bars, final flasking and processing with an injection molded acrylic resin (Fig. 15).
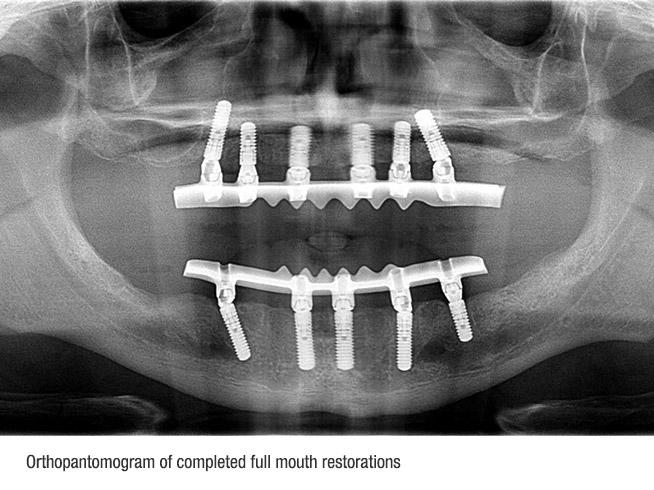
The final hybrids were delivered to the patient and occlusion was again adjusted and verified using a T-Scan (Fig. 16). An orthopantomogram of the completed treatment verified ideal implant healing and fit of the final CAD/CAM titanium bars (Fig. 17). The patient's post-operative clinical result revealed a patient who was extremely pleased with the process and the definitive outcome (Fig. 18). "I can't believe I was able to get my all teeth back and I never once wore a denture!” exclaimed the patient. "I can comfortably eat again and my teeth have never looked better!”







Scott E. Keith, DDS, MS
Board Certified Prosthodontist
1111 Civic Drive #320
Walnut Creek, CA 94596
925-935-4040
925-935-4077 Fax

John J. Petrini, DDS, MS
Board Certified Prosthodontist
1111 Civic Drive #320
Walnut Creek, CA 94596
925-935-4040
925-935-4077 Fax