The rehabilitation of edentulous maxillae using the Straumann Pro Arch concept
submitted by:
Memhet Akif Eskan, DDS, PhD
Cemil Kavrayis CDT
Murat Cil CDT
Share This


Memhet Akif Eskan, DDS, PhD
Cemil Kavrayis CDT
Murat Cil CDT
Share This
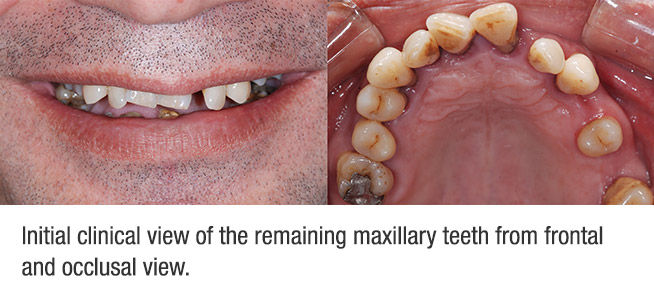
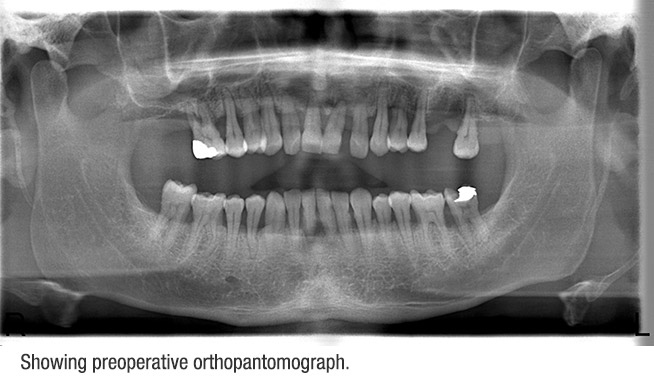
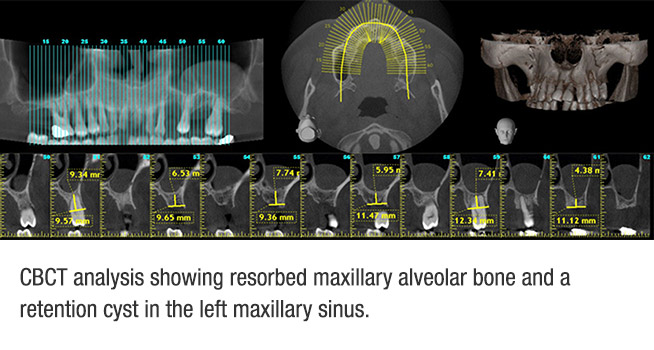
A 42-year old male patient in good physical health required a dental treatment. He reported that he was a former smoker and did not take any medication. He complained that his upper teeth were getting loose and he was unhappy with his aesthetics. Following his clinical (Fig. 1) and radiological examination (Fig. 2), it was decided that his remaining upper teeth prognosis was hopeless. At the lower jaw, 23 through 26, 28 and 31 prognosis were hopeless too. The remaining lower teeth prognosis was fair. Plaque, and gingival index were 90% and 2.5, respectively. In radiological exam, we observed more than 70% of horizontal bone loss in the maxilla and 23% through 26% in the mandible (Fig. 2). Furthermore, CBCT analysis showed that there was a rounded and dome-like lesion in the left maxillary sinus (Fig. 3). Following a consultation with an ENT, it was diagnosed as a retention cyst of the maxillary sinus, which may show 17% to 38% spontaneous regression and disappearance.
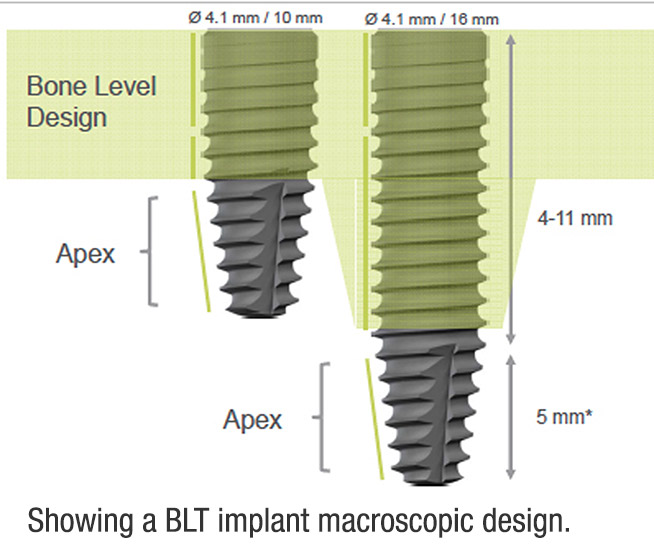
Due to the hopeless prognosis of the maxillary remaining teeth, all upper teeth were planned for extraction. The patient will not tolerate a removable prosthesis in the maxilla at any time during treatment. The patient requested a fixed restoration throughout the treatment time. In order to meet the patient’s request and shorten the treatment time, a screw-retained provisional prosthesis was planned following extractions and implant placement at the same time in the maxilla. Four implants, of which the two posterior implants were tilted, were planned to be placed in the maxilla. Since our goal was to load implants immediately, the implant’s primary stability had to be established for immediate function. However, primary stability may become an issue especially in the soft bone, which may be handled by macroscopic implant design, such as a tapered implant tip (Fig. 4 BLT implant). This modification may result in enhanced mechanical anchorage of the implant at the placement, allowing for immediate loading.
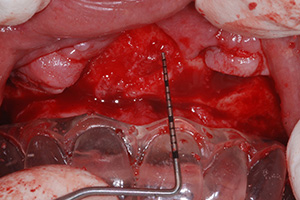
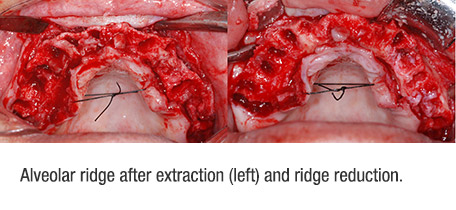
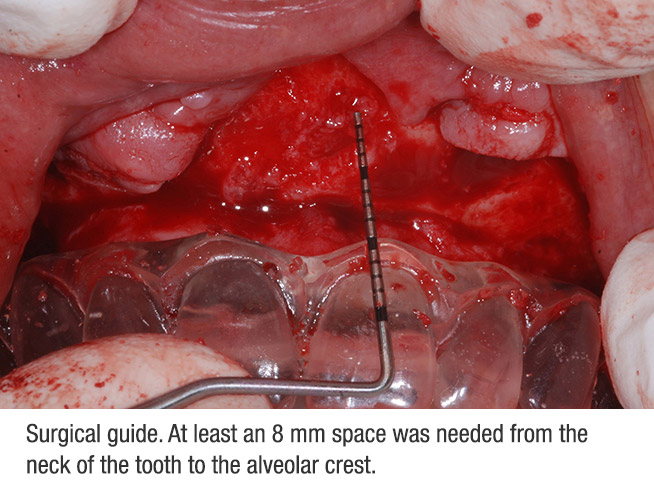
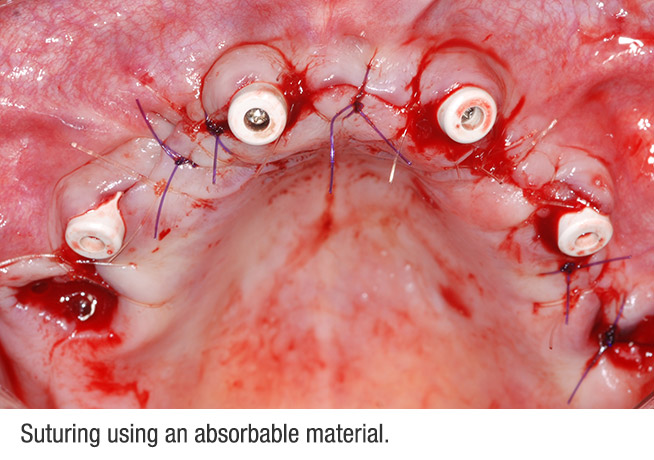
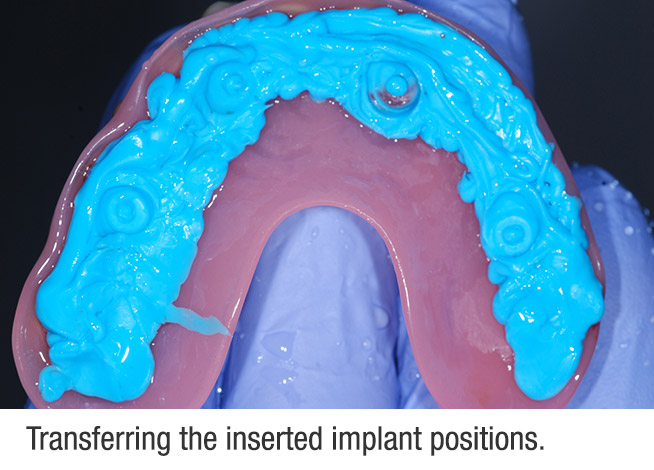
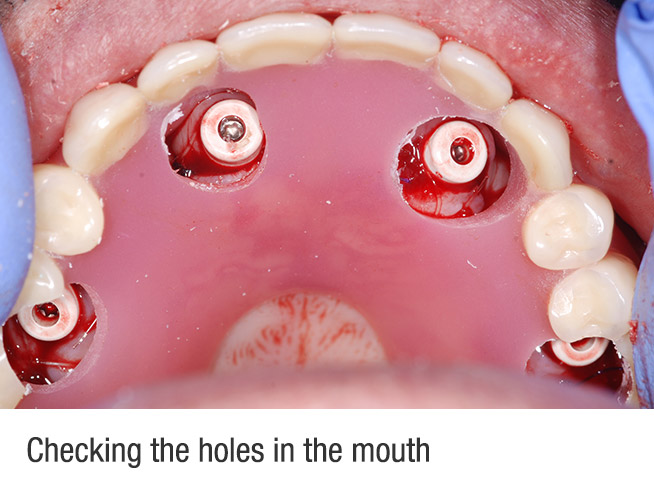
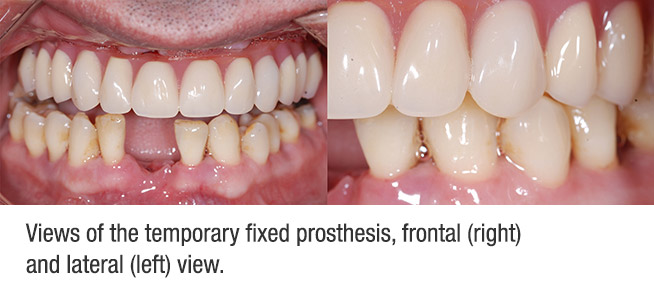
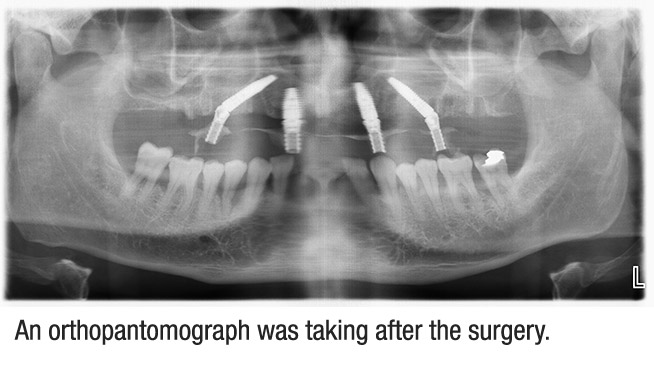
The surgical procedures were carried out under local anesthesia with articain hydrochloride (40 mg/ml in 1.7 ml). The patient was prescribed an antibiotic (amoxicillin + clavunic acid) one day before the surgery and continued for one week. NSAID (ibuprofen, 800 mg) was given on the day of surgery and daily for five days postoperatively. Following reflection of a full thickness flap, the remaining upper teeth were extracted and all granulation tissues were removed (Fig. 5). One of the most critical steps is to manage interocclusal space. Inadequate bone removal may result in esthetic issues during prosthetic procedures. A surgical guide was made of clear acrylic, which helped us to determine if there was enough interocclusal space, at least 8mm (Fig. 6). A small window was opened to the sinus with a round bur to locate the medial sinus wall (Fig. 7). Countersinking, when needed, was done to secure both buccal and lingual cortical bone contact at the implant collar in the thin bone crest. Care was taken in the selection of the axial implant length to avoid a conflict with the posterior implants. Usually, the axial anterior implant length is shorter than the tilted implants. The posterior implants were placed with about 45°- 30° of inclination and 30° angulated screw-retained abutments were placed on the posterior implant correcting the angulation for the immediate prosthetic rehabilitation. For the anterior axial implants, 0° SRA were placed and the wound was sutured using an absorbable suture (Fig. 8). Then, the inserted implant position was roughly transferred on the temporary prosthesis using a bite registration material (ImprintTM Bite 3M® ESPE®) (Fig. 9). The opened holes were checked (Fig. 10) before attachment of the temporary abutment on the provisional prosthesis. A provisional full acrylic complete-arch prosthesis using temporary titanium copings was delivered on the day of surgery. The provisional prosthesis was screwed into the patient’s mouth, the patient’s smile was checked (Fig. 11) and an OPG was taken (Fig. 12). In terms of oral hygiene, the patient was instructed to use cholorhexine for the first week then recommended to use a water pick. The patient also was instructed to eat a soft diet for 6 weeks post-operatively.
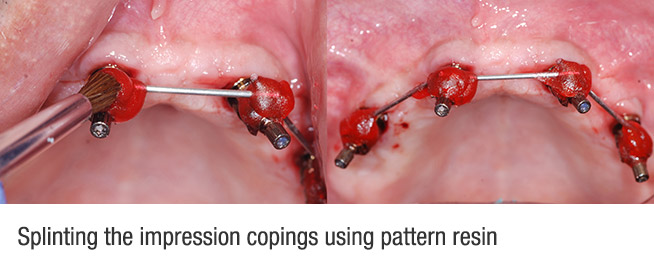
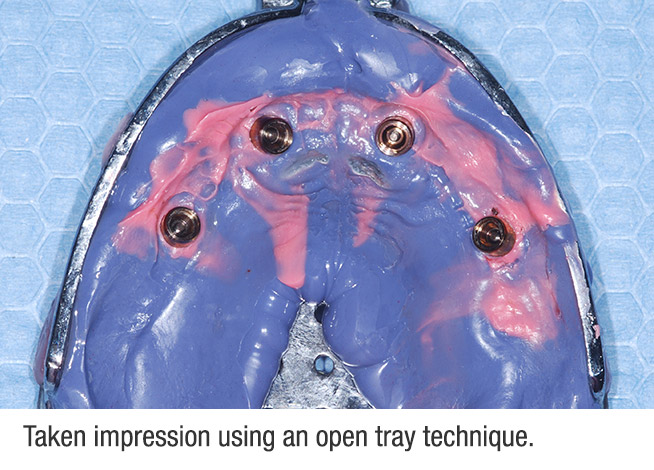
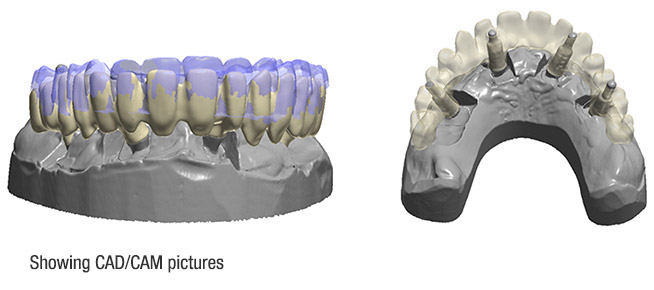
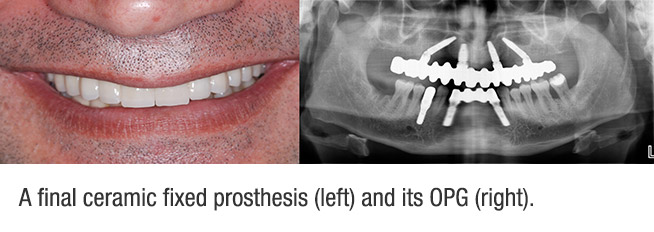
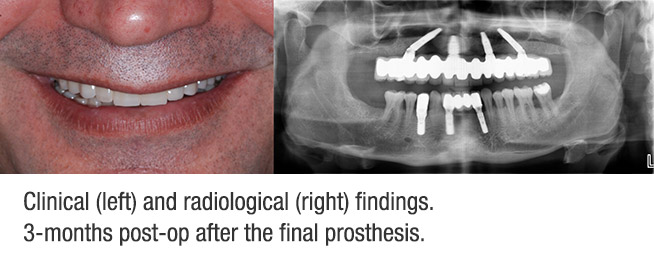
After four months healing time, the provisional prosthesis was removed (Fig. 13). All implants fulfilled: 1) stable when tested manually and 2) no sign of peri-implantitis at the clinical and radiological exam. Before the impression, all implants were splinted to each other using pattern resin (GC®, America Inc) (Fig. 14) to avoid any unpredictable distortion. Then, an open tray impression was taken using polyether siloxane (3M® ESPE) (Fig. 15).Using the plaster model, the provisional was seated on the model to see if the impression was taken correctly. Since the patient was happy with the esthetic provisional prosthesis, it was scanned (Fig. 16) for a CAD/CAM framework. Following all try-ins, including metal and porcelain, the prosthesis was delivered (Fig. 17). The patient was appointed for the first 3-month re-call. The final prosthesis clinically was functional and radiologically showed no bone loss (Fig. 18).
The overall functional and esthetic outcome of the treatment was judged excellent by the patient. Seven months after the initial loading, no crestal bone loss was observed around the implants. This case report showed that a resorbed endentulous maxilla with various types of bone quality could be restored with good function and esthetic using immediately loaded implants featuring a narrow apex. Favorable marginal bone level/s were maintained by the inserted BLT implants.


Memhet Akif Eskan, DDS, PhD
Diplomate, American Board of Periodontology
Clinic Eska, Private Practice, Instanbul, Turkey

Cemil Kavrayis CDT
Kavrayis Dental Lab, Istanbul, Turkey

Murat Cil CDT
Kavrayis Dental Lab, Istanbul, Turkey